
Bilgin et al observed 518 patients with keratoconus who wore contact lens over a 30-year period, indicating that wearing contact lens is the most common and successful management measure for keratoconus, it can provide patients with good vision and control keratoconus progression, and wearing contact lens delayed the need for surgery in 98.9% of cases. The contact lens acts on the tear film layer of the patient to create a new regular anterior surface in front of the optical system, and the irregular cornea is covered, so as to correct the aberration caused by the irregular surface, improve the patient's vision and contrast sensitivity, and significantly improve the visual quality. RGP contact lens has long been used to correct refractive errors and astigmatism caused by irregular corneal surface. This article will review the effect of RGP contact lens on keratoconus progress, and provide reference for clinical application of RGP contact lens.
The mechanical friction and inflammation caused by direct contact between RGP contact lens and anterior corneal surface, poor follow-up compliance of patients, and the improper management of RGP contact lens will cause damage to the morphological and biological characteristics of each layer of eye structure, and further affect the visual quality and disease control of keratoconus patients.

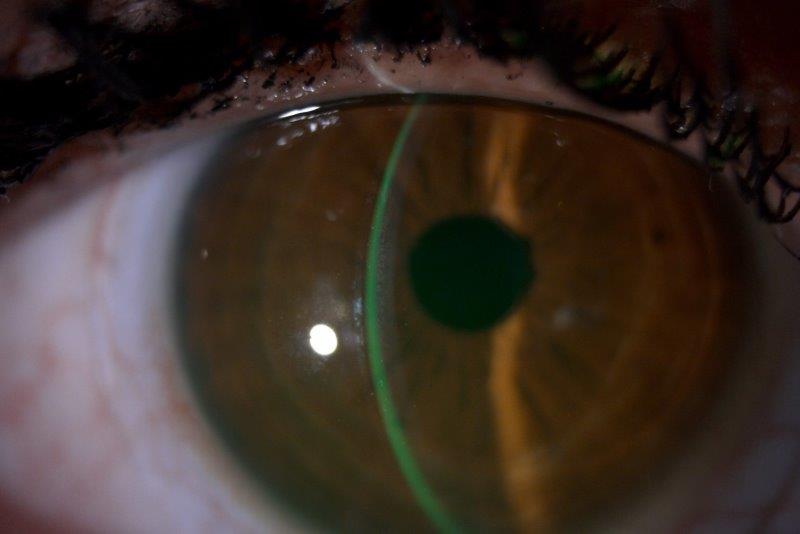
Although the benefits of RGP contact lens are widely recognized, knowledge of complications is now evolving with increased numbers of wearers. Patients wear RGP contact lens to form a “contact lens-tear-cornea” system to correct irregular astigmatism, reduce aberrations, provide good visual quality, and control the development of the disease through mild “shaping” effect. RGP contact lens is designed from a special rigid hydrophobic material. Suspected factors include genetic and environmental factors (eye friction, contact lens wear, ultraviolet exposure), allergic diseases, specific diseases and inflammation. The mechanism of keratoconus has been studied for a long time, and it is generally believed that keratoconus is the result of multi-factor and multi-pathologic process. In this paper, we mainly discuss this type. Among them, corneal RGP contact lenses are the first choice for patients with keratoconus and are widely used, which is often referred to as RGP contact lens. According to the total diameter, RGP contact lens can be classified as corneal contact lens, intralimbal contact lens and scleral contact lens. There are a variety of contact lenses available for keratoconus management, such as rigid gas permeable (RGP) contact lens, soft and soft toric contact lens, piggy back contact lens, hybrid contact lens, scleral and corneoscleral contact lens. The use of contact lens is an important non-operative management measure for keratoconus. At present, there is no cure for keratoconus, improving the visual acuity and delaying the development of the disease are the main clinical intervention purposes. The central part of the cornea protrudes forward in a conical shape, resulting in highly irregular myopic astigmatism and visual impairment. Mayo Clinic's eye experts are highly experienced in treating people with scleral lenses.Keratoconus is a chronic progressive disease characterized by thinning and expansion of the cornea. Lenses can be customized for each person.


The lack of contact between the back of the scleral lens and the cornea reduces pain, and the spherical front surface of the lens improves vision. A fluid barrier keeps the scleral lens from touching the cornea. A scleral lens differs from a standard contact lens - it's larger and rests atop a layer of tissue over the white part of the eye (sclera). Scleral contact lenses can help people who don't respond to other treatments for their cornea conditions.


 0 kommentar(er)
0 kommentar(er)
